Updated 7/2023
1. FUNCTION
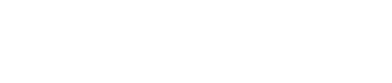
Hip resurfacing creates the most normal artificial hip joint possible.
This is most important for the athletic person who wants to return to impact sports or who wants to do heavy physical work. But even at fast walking speeds hip resurfacing gait is more normal than gait with a total hip replacement.
This is the real and over-arching reason to choose hip resurfacing instead of a standard stemmed total hip replacement (THR). The central problem in a hip with severe arthritis of any type is that the 3mm surface layer of hyaline cartilage on both sides of the joint is worn away. This is sometimes called a bone-on-bone joint. It is not yet possible to reestablish this natural hyaline cartilage.
Microfracture during hip arthroscopy can stimulate fibrocartilage to heal small defects. Sometimes this helps, if the defect is tiny, but in defects more than 1cm2 it rarely results in a happy hip. If the bone is not covered with hyaline cartilage, the pain receptors in the bone are stimulated, especially during weight-bearing and impact activities.
Stem cell injections are also not able to regrow this cartilage and are therefore ineffective in solving the problem in severe arthritis. Depending on the pain tolerance of the patient and their willingness to limit vigorous activities, sometimes medications and injections of various types can help them live an acceptable life for some time. But cartilage never regrows – the process of cartilage loss is typically progressive. Sometimes patients become debilitated within 6 months, but usually, the problem progresses for a few years before patients become convinced that an operation is their best option.

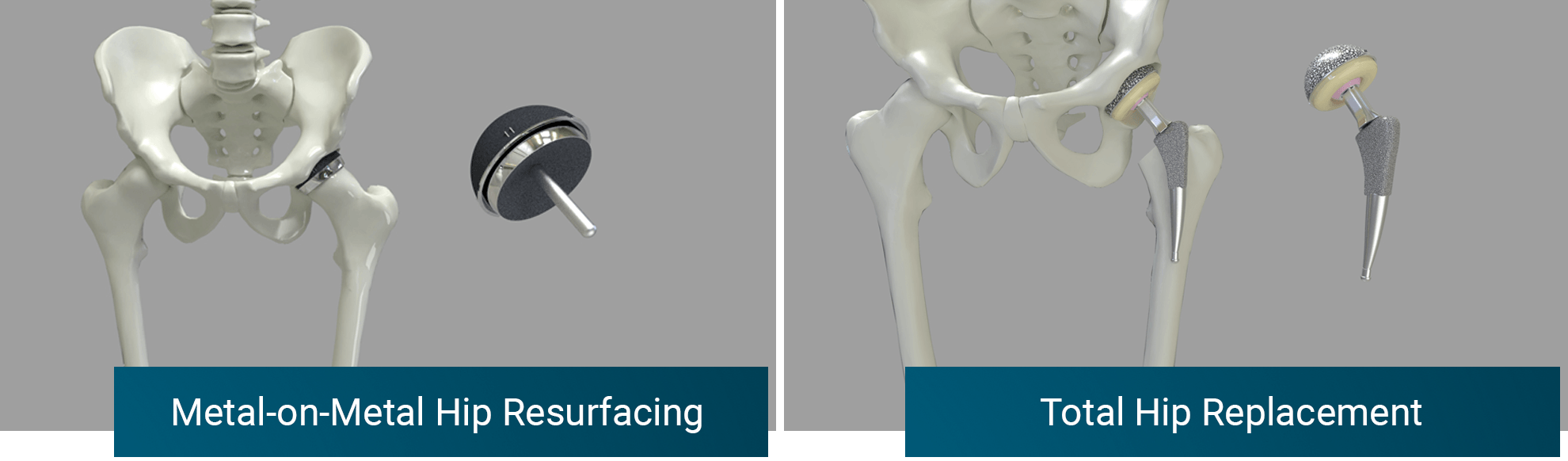
Joint replacement is the only adequate way to address severe cartilage loss. The basic principle is that the remaining cartilage and some bone on both sides of the joint are removed and replaced with an artificial surface. This surface must be solidly attached to the bone on either side of the joint. After this, when the joint moves, the artificial surfaces are rubbing on each other, and the bone behind them is again protected as in the original joint with hyaline cartilage.
But an artificial joint is never “normal”. Surgeons cannot create “normal”. Imperfect healing of the soft tissue envelope (muscles ligaments and tendons) that the surgeon must pass through as well as the biomechanics of the artificial joint itself determine residual symptoms. Many claims are made about the healing process for the method of “approaching” the joint, that cannot be verified. In recent times an “anterior approach” for THR has gained many surgeon proponents who claim that recovery is faster and better with this approach. This has not been verified with scientific data. In analyzing the large sum of published papers on this topic, it does seem likely that the dislocation rate using small bearing THR is lower from the anterior rather than the posterior approach, but the femoral fracture and infection rates seem to be higher. It is a wash. The surgical approach cannot be demonstrated to affect the final outcome of THR.
However, Hip Resurfacing Arthroplasty (HRA) has been demonstrated in numerous controlled studies to lead to a more normal hip than a THR. This is likely due to the fact that a more biomechanically normal hip is created with the resurfacing operation. The hip is reconstructed closer to its normal state. Only a thin layer of bone on either side of the joint is sacrificed, and the final bearing size is virtually the same as the original hip. About 4mm of bone on both sides of the joint is replaced with metal. The resulting artificial joint has near normal stability once the ligaments heal and load is transferred near normally to adjacent bone.
In a THR, on the other hand, a similar amount of bone is removed from the socket, but it is replaced with a much thicker 2-piece implant (metal shell and bearing liner) that results in a downsizing of the artificial bearing size compared with normal. This has two consequences. First, the head cannot be whittled down enough to place an artificial surface that will fit in this smaller bearing cup; it must therefore be completely removed and replaced with a smaller head sitting on a stem. The stem is a large piece of metal that completely fills the femoral canal for 4-10 inches. The second consequence is that the smaller bearing size is not as stable as the original natural joint. This will be discussed further below.
Although instability is a big problem for THR, the main problem that limits high activity levels after THR seems to be the stem. This mainly affects people who wish to participate in impact sports. In some ways, the stem provides a Safety Device for a THR, because it prevents patients from being able to participate in high-impact activities and thereby 'protects' the THR from failure to some degree. Some THR surgeons counsel their patients to resume any activity that they desire even though it is well-known that THR fails faster the younger or more active the patient is. Most surgeons do advise limitations to high impact. But even without these surgeon-imposed limitations, most patients are unable to perform high-impact activities.
Patients who desire to return to such activities are routinely described by their surgeons as having “unrealistic expectations”. But high impact is routinely possible with HRA and does not result in any higher failure rate with HRA. The reason THR patients cannot adequately perform impact activities is the stem. The HRA stem is tiny and is NOT load-bearing. The force applied to the HRA head is transferred directly to the surrounding remaining femoral head bone in a near-normal fashion.
The THR stem is large, canal filling, and transfers load to the femoral shaft. This is very unnatural and the body doesn’t like it. The result is thigh pain. Most THR patients are improved (although 20% have been shown to have at least moderate residual “unexplained” pain), but thigh pain of at least a slight degree occurs in 30% of patients even with light activities of daily living (ADL). 3-5% have moderate or worse thigh pain with ADL. In gait lab analysis THR and HRA patients alike walk normally at slow gait speeds. At a fast-paced gait, the THR patient unconsciously shortens his gait and shifts load to the other hip. The HRA doesn’t. This likely means the stem is bothering people to some degree even at fast walking speeds. Impact sports cannot be analyzed in a gait lab. Routine hip follow-up questionnaires that we use do not set a very high bar, therefore THR and HRA seem similar in many studies that use these methods. If standardized “sport activity” questionnaires are instead utilized, HRA patients are much more likely to enjoy impact sports.
A hip resurfacing looks much more like a normal hip and scientific evidence demonstrates that it functions more like one. This is obvious to most patients who understand how they differ. The question I have is why so many surgeons fail to see this and persist in giving young patients THR and then pronounce them “unrealistic” if they want to play sports but are unable to do so. On the other hand, THR is reliable and makes most people better. Old folks who think an “active lifestyle” is golf and walking on the beach are usually satisfied with THR. But younger patients who still want to participate in extreme motion or high-impact activities are much better off with an HRA. It is the closest thing to a normal hip that surgeons can create. Patients are almost never limited in any activity by their hip after 1 year.
The only “expectations” that I need to set for my patients is for long-distance running. I have found that this is the single most demanding activity for the hip. I have many patients who run distances regularly including triathlons, marathons, and even ultra-marathons. I allow this starting at 6 months. Even this extreme activity does not result in a higher failure rate. But it is not always possible. Some patients still have hip pain after 2-3 miles of running and are therefore disappointed. These patients can typically perform all other extreme sports (such as basketball, soccer, or singles tennis) or exercise programs (P90X) that they like, but are unable to distance run. The x-rays and ion levels are excellent. The cause of the pain is “unexplained”. We can speculate that stress transfer from implant to bone is not normal, tissue healing is not perfect, or even that the hip pain is “referred” from the back. Some patients can work through this with persistent progressive weekly running on a soft surface. Others have to shift to other exercises such as cycling.
Even though HRA is an imperfect copy of the original hip, it is today the closest a patient can come to a normal hip. I cannot promise a return to distance running; on the other hand, even distance running does not result in a higher rate of implant failure and I encourage it.
2. DURABILITY
Hip resurfacing is more durable in any patient, any age, sex, implant size, or diagnosis.
This is more important the younger that you are because THRs fail faster in younger patients, and these patients need them the longest. People over 70 will probably not outlive a THR.
My current implant survivorship is 99% at 17 years. A large multi-center international study of hip resurfacing experts has demonstrated that in the hands of dedicated hip resurfacing arthroplasty (HRA) surgeons, the 10-year implant survivorship is 95% and the twenty-year implant survivorship is 90% in the most demanding young patients (age <50).
Joint Registries show a benchmark implant survivorship of approximately 95% at 10 years for total hip replacement (THR) (mean patient age 70). The failure rate increases with decreasing patient age. In patients under 50 years, the 10-year implant survivorship is only 80% with THR and the twenty-year survivorship is 50%.
In the British registry, HRA carries a benchmark implant survivorship of 92% at 10 years. HRA patients tend to be younger, therefore this is similar to age-matched THR patients. But most HRA in Britain is performed by surgeons doing this operation only 1-2 times per year. Most surgeons have much more experience performing THR. As a result, registry data for HRA are “contaminated” with results from inexperienced surgeons and results are therefore negatively biased against HRA.
In the Australian registry, men younger than 60 have better implant survivorship with HRA than THR, all other groups have better implant survivorship with THR. This has led many surgeons to proclaim that HRA should only be done in men under 60. But interestingly these same surgeons don’t recommend that THR should not be done in men under 60. Implant survivorship in registries is often overvalued as a means of choosing the best implant or operation. Registry data provides a benchmark for what the average surgeon can achieve. It might be better to choose a surgeon who can provide data that outperforms the registry.
HRA is a more complicated operation than THR and requires that a surgeon dedicate extensive time and energy to master it. Few have done this. After 1000 cases of any specific operation, most surgeons could be considered true experts. The multicenter HRA study demonstrates that surgeons dedicated to HRA can far surpass the implant survivorship benchmark of THR in younger patients. With my 99% 17-year implant survivorship, I have demonstrated that I can far surpass the registries and all expert surgeon series for all patients regardless of age, sex, or diagnosis.
In most studies of THR there is minimal difference in durability between the sexes. In most HRA studies women achieve lower 10-year implant survivorship than men. In my outcomes, this was true until 10 years ago when we managed to equalize the results.
For the diagnoses of osteonecrosis and dysplasia the durability is lower than for osteoarthritis for both THR and HRA. In my HRA outcomes, this was true until 10 years ago when we managed to equalize the results. Currently, my 10-year implant survivorship stands at 99% for all patient categories.
-
Summary
-
10-Year Implant Survivorship
- HRA
- Dr. Gross (any age, sex or diagnosis)
- 99%
- Intl. multicenter study (mean all patients under 50)
- 95%
- Men:
- 99%
- Women:
- 93%
- British registry (mean all patients)
- 92%
- THR
- British, Australian, Swedish registries (mean age 70)
- 95%
- Swedish registry (patients under 50)
- 80%
Implant survivorship is a statistical way to report how long an implant or operation is likely to last. If a surgeon (or registry) has data on when each operation was done and, on the dates, that all failures occurred as well as data on when patients have deceased, implant survivorship can be calculated using the Kaplan-Meier method. The estimate is only good for the number of years that have passed since the first operation was performed. This gives an estimate of how long an implant is likely to last. Registry results give average surgeon performance, individual data is required to determine how each surgeon performs compared to the average. If a surgeon tells you that a certain hip operation will last twenty years this is pretty meaningless. Most hip implants being put in today do not have any 20-year data to support such a claim. They need to tell you the odds of lasting 20 years and based on what data this estimate is made.
Please keep in mind that registry data represent an overestimate of actual implant durability. This error becomes greater as the study cohort of patients ages. This is because only failures that lead to revision are actually counted as failures by the registry. In a National Health System where waiting times for surgery are sometimes several years, the years a patient waits for revision count as “successful” years. If a patient elects not to have revision surgery, their case still counts as successful; this is more likely in older patients with more comorbidities.
3. HIP STABILITY
Hip resurfacing has a lower rate of dislocation.
This is important for all patients, but particularly those that wish to engage in extreme motion activities such as yoga, ballet, and kayaking.
Dislocations in my series of 7000 hip resurfacing arthroplasties (HRA), dislocation has occurred in 0.3% of cases. Of these, 0.1% have had recurrent episodes of instability and require another operation to correct the problem. The international HRA study has very similar data. Most dislocations occur in the first 6 months, thereafter it is exceedingly rare.
For total hip replacement (THR) the instability rate is about 3% but varies highly. About 1-2% require revision for recurrent instability. Unlike HRA, Risk persists throughout life. There are several risk factors for dislocation:
- Bearing size: The standard THR bearing is from 28mm- 36mm. The larger the bearing size the lower the risk of dislocation, but the higher the risk of trunion corrosion.
- Approach: The anterior hip approach is associated with a lower risk of dislocation, but carries a higher risk of femoral fracture and deep infection.
- Patient Factors: women, older patients, those with neurological deficits, and those with dysplasia carry a higher risk of dislocation.
Natural bearing sizes vary from 40mm to 60mm. The average woman has a bearing size of 46mm, and the average man has 52mm. HRA restores these natural sizes and results in a dislocation rate of 0.3%, while THR bearing sizes are usually 28-36mm and result in a dislocation rate of 3%. THR creates a biomechanically abnormal hip that is inherently unstable. Most of the HRA dislocations occur during the initial soft tissue healing process (6 months) and are due to patients failing to follow instructions. Once the tissues are healed, all restrictions are lifted with HRA, and all extreme bending activities such as yoga, kayaking, and ballet are allowed. In THR, the hip is always unstable and extreme positions anytime throughout the patient's remaining life put them at risk for dislocating.
It is well-established that the smaller the artificial bearing size compared to the patient's normal is, the higher the risk of dislocation. A larger bearing size in THR requires a thinner 2-piece cup. In the past, this led to high rates of plastic wear failure (plastic becomes too thin). With modern antioxidant-stabilized cross-linked polyethylene (VE XLPE) the wear problem has largely been solved and thinner 2-piece cups are more durable. But another problem has surfaced: trunion corrosion. The larger the artificial head, the greater the stress on the connector to the stem (trunion) and the higher the chance of a trunion corrosion failure. Current estimates are that this may occur in 1-5% of THR within 10 years. We still do not understand this problem well and therefore cannot design a solution. Therefore, in THR, the smaller the ball the higher the dislocation risk, but the larger the ball the higher the trunion corrosion risk. Even the largest balls do not approach the patient's natural bearing size. Only HRA can create an artificial joint with near-natural stability and no possibility of trunion corrosion.
But a resurfaced hip is not totally normal. An HRA is more stable than a THR even before any healing occurs. But until the muscles and ligaments that we have cut and repaired have had a chance to heal, position precautions are required (6 months). Rare dislocations after this time may be due to the fact that in some patients, the soft tissue healing process has failed in some respect, or simply due to the fact that the central ligamentum teres has been removed (in every THR and HRA) and that hip stability is not quite normal. But from a practical standpoint, hip stability in HRA is near normal at 6 months postop and virtually all range of motion restrictions are lifted. Only a few extreme yoga and ballet positions should still be avoided until 1 year after surgery.
4. BONE PRESERVATION
Equal socket bone is removed but less femoral bone is removed with HRA.
Most important for the younger patient who is more likely to require revision surgery in their lifetime.
If the hip arthroplasty (THR or HRA) has failed, one or both implants have to be removed and replaced by new ones (revision). There is always bone loss associated with implant failure and/or removal. On the socket side, this is the same for both HRA and THR. On the femoral side, there is a distinct advantage for HRA. HRA femoral failures require revision to a stemmed THR, but the standard femoral neck cut that is done for primary THR is all that is required. An HRA femoral revision is no different than a primary (1st time) femoral stem for a THR. A revision of the femoral side of a THR usually involves much more surgical time, blood loss, and bone damage. A longer stem is then used to reconstruct.
If all else is equal, it is always better to preserve your bone for the future.
5. LONGER LIFE
10-year patient survivorship is 20% better for HRA patients.
For patients matched for age, sex, diagnosis, economic status, and medical comorbidities there is a 20% lower mortality in the HRA group than the THR group. The best study was an analysis of the British Registry data by Kendall from Oxford University. It has been confirmed in another independent analysis of the same data as well as by data from the Australian Registry.
Calculation of implant survivorship was explained above. We are discussing patient survivorship here. In large population-based studies, the survivorship of patients who have had a THR is about the same as those that haven’t. When HRA is compared to THR in a controlled fashion, fewer deaths occur in 10 years in the HRA group. The first impulse is that HRA patients are generally younger – so this makes sense. But these studies have controlled for age as well as many other factors that might explain the difference.
The mean age for an HRA patient in my practice is 54 years. Using very approximate numbers, if the chance that anyone of this age will die within 10 years is about 5%, then the person who has an HRA has a 20% lower incidence, which means 4% rather than 5%. These are small but strongly statistically significant numbers from a very large database. The only explanation I can hypothesize is that HRA patients are more able or likely to exercise than THR patients. Regular and vigorous exercise promotes longevity. More importantly, this data helps to dispel the concept that many total joint surgeons promote, that metal ion release from hip resurfacing implants is a significant health risk.
6. LOWER ODDS OF DEBRIS FAILURE
Hip resurfacing now has a lower chance of debris failure than total hip replacement.
Excess wear or corrosion debris can cause failure due to tissue irritation. In HRA, the problem is wear due to a malpositioned cup (risk 0/4000 in the last 12 years). In THR, the problem is corrosion of the trunion of the head/neck connector (risk 1-5% by 10 years).
The last wear failure I experienced was a hip resurfacing arthroplasty (HRA) implanted in 2009, over 4000 cases ago. HRA does not have a trunion to corrode. In total hip replacement (THR), wear failures have been extremely rare in the last 10 years with the use of improved plastics (antioxidant stabilized crosslinked polyethylene), But failures due to trunion corrosion in THR have become more common, resulting in 1-5% failures by 10 years. Both wear failures in HRA and trunion corrosion failures in THR are mainly caused by extreme tissue irritation of the resultant debris.
The reason many hip replacement experts cite to claim THR is superior to HRA is because of failures due to inflammatory tissue reactions to debris. This process has many names such as ARMD (Adverse Reaction to Metal Debris), ALTR (Adverse Local Tissue Reaction), ALVAL ( Acute Lymphocytic Vasculitis Associated Lesion), “ion problems”, “pseudotumor”(false tumor), or “metal allergy”. The terminology is confusing and even scary; these processes are not fully understood by joint surgeons and are often used as a scare tactic to persuade patients to avoid metal-on-metal hip resurfacing. But the problem of inflammatory tissue reaction is now more common in THR than in my HRA. There are several complex and intertwined issues at play here; I will try to explain them.
Any artificial joint replacement is subject to failure due to corrosion, or excess wear. All corrosion/wear debris has the opportunity to cause soft tissue or bone irritation and damage as well as pain. A small amount of debris is well tolerated by most people. If the amount of debris gets too large, soft tissue irritation, muscle damage, and bone loss can occur. How does debris cause tissue irritation?
Allergy is not a cause of failure. It is likely that some people are more sensitive to debris than others, but “allergy” to internal metal or plastic particles does not seem to occur. For example, skin rashes to nickel touching the skin (cheap jewelry) occur in about 20% of the population and can be verified by a skin patch test. People who have a positive skin patch to nickel are not more likely to suffer residual unexplained pain or frank implant failure in joint replacement surgery. Cobalt chrome alloy contains a trace amount of nickel and there is a pervasive belief that implants made of this alloy can result in failure in “allergic” patients. Skin patch studies refute this hypothesis, but it persists. Others claim that a Lymphocyte Transformation Test (LTT) is a better way to asses allergy than skin patch tests. There is no validation of this blood test for this purpose. We attempted to validate this hypothesis and found the LTT done before surgery to be unable to predict patients with unexplained pain or implant failure. Allergy has never been demonstrated as a plausible cause for failure by any scientific study. My interpretation of the problem is as follows.
Joint replacements don’t recreate totally normal joints. Most patients with really bad joints feel vastly improved. But having some residual symptoms is “normal”. Certain failure modes or causes of residual pain are understood; these causes of failure are “explained” and can sometimes be corrected or improved with further surgery. Causes for residual pain after joint replacement continue to be discovered, but many are elusive and may be discovered with time. Unexplained residual pain is seen in 30% of the total knee, 20% of the total hip, and 2% of my HRA patients. When a patient has “unexplained” pain, “allergy” is often used to explain the cause. One danger is that some surgeons recommend risky revision surgery to resolve the unproven “allergy” when no evidence exists that this will work.
Some causes of residual pain are inherent in the operation. For example, residual thigh pain in stemmed THR is a major problem for many patients who wish to participate in high-impact activities and a less common problem for those satisfied with regular activities of daily living (ADL). It is caused by abnormal stress transfer from a stiff THR stem to a more flexible surrounding femoral bone. There is no solution to this problem. The prevention is to perform an HRA instead. 30% of THR patients experience at least some thigh pain, and 3-5% have moderate to severe thigh pain. Impact sports are limited by this problem
Metallosis is a real problem. Unlike “allergy”, there is a strong body of evidence that helps us understand the cause, solution, and even prevention of this problem. Metallosis can also be called adverse wear-related failure (AWRF). It is caused by overloading the hip with cobalt-chrome wear debris. Again, a small amount of debris is well-tolerated, but excessive debris irritates the tissue causing pain and it can gradually damage muscle and bone. This requires revision surgery. If done by an expert, the success of the revision is similar to any other revision. We have published a 96% 8-year implant survivorship for HRA revision for any cause. Permanent severe muscle damage crippling the patient has been reported by some centers for AWRF revision. I would suggest their high failure rate is due to inexpert surgical technique.
Cobalt-chrome (CC) metal-on-metal (MoM) bearings exhibit a very low wear rate when tested with fluid lubrication in the lab. In fact, the wear rate is lower for MoM than for metal or ceramic on plastic (MoP, CoP). Only ceramic on ceramic (CoC) sheds less wear debris. All of these bearings shed so little wear debris that tissue irritation should never occur. If the wear rate were the only consideration, CoC would be the ideal bearing choice. But many other factors (beyond the scope of this article) are also at play. Why then do we see metallosis with MoM bearings?
The reason, first discovered by Koen DeSmet and then further elucidated by us, is that edge loading causes excess wear. When MoM implants are “ideally” positioned, extremely low wear results – the implant should never “wear out” in a hundred years. If the socket component is placed too steeply or too anteverted (forward tilt), edge loading can occur. Edge loading occurs when the bearing “contact patch” is too close to the edge of the socket. The main point of contact between the head and socket and its patch of greatest wear in the standing position is called the “contact patch”. The degree of socket tilt (inclination and anteversion) and the tilt of the pelvis in the standing position influence the position of the “contact patch”. If the socket is placed so that the contact patch is too close to the edge of the socket, edge loading is said to occur. When a bearing is edge-loaded, the normal fluid film that the bearing runs on escapes, and the wear rate goes through the roof. Although CC bearings have a lower ideal wear rate than all other bearings except CoC, they are much worse during edge-loading conditions. But other problems are caused by edge-loading: loud squeaking in the CoC and liner breakage in MoP bearings.
Edge-loading is more common when the acetabular coverage arc (depth) is lower. One brand (Depuy ASR) of metal on metal THR and HRA was designed with a much lower coverage arc than all other brands and was therefore much more likely to be implanted in a position to result in edge loading. This was the main reason that the DePuy ASR had a disastrous 30-50% five-year failure rate. Small implant sizes in all brands have lower coverage arcs than larger bearing sizes; this explains the higher AWRF rate in women.
This problem has 3 possible solutions. Taking smaller implant sizes off the market (BHR), changing socket design to equalize coverage arc on all implants to 165º (Conserve plus), or learning to implant all sizes in a safe position to avoid edge-loading. The latter has been my solution.
After Koen DeSmet noticed that AWRF in HRA occurred more commonly in women with steep cup positions, we began to study this further. In 2013, we published a paper based on an analysis of over 700 cases. We were able to calculate a “safe zone” for socket position which avoided AWRF. This safe zone was named RAIL (Relative acetabular Inclination Limit). A “safe zone” to avoid edge loading exists for all implants, but the size of the zone increases with increasing bearing size. While we were working on this paper, we also worked on techniques to make sure that the socket component could be placed within this safe zone.
By 2009, we were able to develop an intraoperative x-ray technique called NSIOR (normalized to standing intraoperative radiograph) that allowed us to be certain that every single patient (including for smaller bearing size) could be implanted within the safe zone. The last socket that was too steep was in 2009. No further AWRFs have occurred in the 13 years since that time; I have performed over 4000 HRA since then. We then followed up with another study published in 2019 verifying that 100% of 2500 consecutive cases could be placed within RAIL and that this would in fact prevent AWRF. This study “validated” the RAIL safe zone that we had created previously with an entirely new set of patients.
Problem solved. AWRF no longer occurs in HRA if the RAIL safe zone is respected. Meanwhile, trunionosis in THR is a cause for failure in 1-5% of cases by 10 years and no solution is in sight.
Why Minimally Invasive Surgery?
With a minimally invasive 4-5 inch posterior approach, minimal blood loss, and multimodal pain management, outpatient surgery is possible. This is more convenient, pleasant, and less costly. Since 2012, we have perfected this outpatient approach for all joint replacement procedures, and over 80% of my operations are done this way. Local patients return directly home on the day of surgery, and out-of-state patients stay in a hotel for 1-2 nights before traveling home. Patients with certain major medical comorbidities, uncooperative insurance plans, or those without capable caregivers are still done at the hospital with a one-night overnight stay. I strongly recommend against staying at rehab facilities unless a patient cannot arrange any support at home.
Accurate X-ray Based Component Positioning
The most critical factor in consistently achieving excellent outcomes in resurfacing is accurate acetabular component positioning. Adverse (Metal) Wear Related Failures (AWRF) can now be completely avoided, even in higher-risk patients requiring smaller implant sizes, by proper acetabular component positioning. We published the world’s first component positioning guideline that is supported by data. We named it RAIL – Relative Acetabular Inclination Limit. We then developed intraoperative X-ray techniques that allow us to achieve RAIL in every case. We monitor all patients for excessive wear using blood ion levels. As a result, we have not created a single AWRF since 2009 (10 years, >4000 cases). Prior to 2007, the rate was 1% at 10 years.
Why Uncemented Implants?
All HRA use uncemented bone-in growth fixation on the socket side. Most brands including the BHR are cemented on the femoral side. We have demonstrated that uncemented fixation on the femoral side gives superior results to cement. Cement is a brittle acrylic material that heats up during implantation (polymerization reaction) burning the femoral head and increasing the chance of early femoral failure. It also is subject to fatigue failure over time resulting in implant loosening type failure.
With uncemented femoral components, we have had a 100% bone ingrowth rate. 0.4% fail due to neck fracture or head collapse, only 1/5000 has come loose since 2007. My femoral loosening rate with cement was 1% by 10 years when I used cement before 2007. We can demonstrate no difference in the early femoral failure rate between cemented and uncemented femoral implants. The difference in late loosening between cemented and uncemented femoral is 1% vs 0.05% at 10 years, this is statistically significant.
Is Resurfacing Safe in Women?
Yes. Durability is equal to men in the last 10 years. Early data from many centers indicated that women had a higher risk of failure due to femoral neck fracture, failure of acetabular ingrowth, and adverse metal wear-related failure (AWRF) than men did. I have data to show that I solved all of these problems at least 10 years ago. Ten-year implant survivorship in women is now 99%; it is now equal to that in men. Femoral neck fractures are rare (0.2%). A trispike acetabular component introduced in 2007 has eliminated the acetabular component failures in deformed dysplasia sockets (90% of dysplasia occurs in women). Understanding proper acetabular component positioning has allowed us to implant acetabular components to avoid AWRF (no new cases since 2009).
Solving the Problems of Revision Failed Resurfacings
Our published results are nearly as good as for primary surgery. Others have also published excellent results for revision hip resurfacing. Most reports on revision for the problem of adverse wear-related failure (AWRF), however, are poor. The worst report is from Oxford, with a 50% short-term failure rate. We have experienced a 100% success rate for AWRF by revising these failures with new large metal bearings placed correctly according to new implant positioning guidelines that we have developed.